Healthy Eating As You Age: Know Your Food Groups
December 29, 2025Healthy Eating As You Age: Know Your Food Groups
Making smart food choices is an important part of healthy aging. Understanding the different food groups — and how much of each should make up your diet — can help you form a healthy eating pattern over time. This article describes the main food groups and other important nutrients recommended for older adults in the Dietary Guidelines for Americans (PDF, 30.6M). We also provide suggestions for how to fit occasional treats into your healthy eating pattern.
It is important to get the recommended amount of each food group without going over your daily recommended calories. Keep in mind that the amount you should eat to maintain your weight depends on your age, sex, and level of physical activity.
Main food groups
Vegetables
Vegetables come in a wide variety of colors, flavors, and textures. They contain vitamins and minerals, carbohydrates, and are an important source of fiber. The vegetable food group includes dark green vegetables, red and orange vegetables, starchy vegetables, and legumes (beans and peas).
Dark green vegetables include broccoli, collard greens, spinach, and kale. Red and orange vegetables include acorn squash, carrots, pumpkin, tomato, and sweet potato. Starchy vegetables include corn, green peas, and white potatoes. Other vegetables include eggplant, beets, cauliflower, Brussels sprouts, celery, artichokes, green beans, and onions. Legumes include black beans, garbanzo beans (chickpeas), kidney beans, soybeans, and tofu. Legumes can also be counted in the protein foods group.
1/2 cup-equivalent of vegetables equals:
1 cup uncooked spinach
6 baby carrots
1/2 cup cooked kidney beans
1/2 cup broccoli florets
1/2 large (3-inch diameter, 3-3/4 inch long) red pepper
1/2 cup cooked green beans
See more foods in the vegetable group.
Fruits
Fruits bring color, flavor, and important nutrients to your diet. There are so many choices — citrus fruits like oranges and grapefruits; different kinds of berries; fruits that grow on trees, such as apricots, cherries, peaches, and mangoes; and others like figs, grapes, and pineapples.
According to the Dietary Guidelines (PDF, 30.6M), older Americans generally do not eat enough fruit. Adding more fruit to your diet can have significant benefits for overall health. Fruits, like vegetables, contain carbohydrates and provide extra fiber that helps keep your digestive system moving. For even more fiber, eat fruits with the skin on — just make sure you wash all fruits thoroughly before eating. Although 100% fruit juice also counts toward this category, at least half of the fruits you eat should be whole fruits. When purchasing frozen, canned, or dried fruit, choose options that are lowest in added sugars.
1/2 cup-equivalent of fruit equals:
1 small piece fruit, such as a 2-inch peach or large plum
1/4 cup dried fruit
1/8 medium cantaloupe
1/2 cup 100% orange juice
1/2 medium grapefruit
1/2 cup grapes
See more foods in the fruit group.
Grains
Any food made from wheat, rye, rice, oats, cornmeal, barley, or other cereal grain is a grain product. This includes bread and pasta, breakfast cereal, grits, tortillas, and even popcorn. Grains — along with fruits, vegetables, and dairy — contain carbohydrates, the body’s main source of energy.
Read food labels to find grain choices that are low in saturated fat and added sugar. Be especially wary of options labeled “low-fat,” which can be high in added sugar.
At least half the grain foods you eat should be whole grains. Whole grains provide iron and many B vitamins, and they have fiber, too. Examples of whole grains include whole wheat, whole oats, whole bulgur (also known as cracked wheat), and whole cornmeal.
Some grain products are refined, which gives them a finer texture and a longer shelf life but removes fiber and nutrients. Most refined grains are enriched, which means that some nutrients are added back after processing. Examples of refined grain products include white flour, degermed cornmeal, white bread, and white rice.
1 ounce-equivalent of grain equals:
1 slice bread
1 small (2-1/2-inch diameter) muffin
1 cup breakfast cereal (flakes, rounds, or puffed)
1/2 cup cooked cereal, rice, or pasta
3 cups popcorn
1 small (6-inch diameter) corn or flour tortilla
See more foods in the grain group.
Protein foods
Proteins are often called the body’s building blocks. They are used to build and repair tissues, and also help your body fight infection. Your body uses extra protein for energy. Older adults should try to eat a variety of nutrient-dense proteins. Choose lean (low-fat) meats and poultry. Keep in mind that you can also get protein from seafood, eggs, beans, nuts, seeds, and soy products. Protein from plant sources tends to be lower in saturated fat, contains no cholesterol, and provides fiber and other health-promoting nutrients. Plant sources of protein, such as nuts and seeds, have different nutritional value than plant-based meat alternatives, which can be heavily processed and high in sodium.
The Dietary Guidelines (PDF, 30.6M) recommend that you eat 8 to 10 ounces per week of a variety of seafood, not only for the protein but also because seafood contains omega-3 fatty acids, such as EPA and DHA, which are good for your heart. Seafoods that are higher in EPA and DHA include salmon, anchovies, and trout. These seafoods are also lower in mercury, which can be harmful, than other types of seafood.
1 ounce-equivalent equals:
1/2 ounce nuts (12 almonds, 24 pistachios, or 7 walnut halves)
1 tablespoon peanut butter
1/2 cup split pea, lentil, or other bean soup
1/4 cup tofu
1 egg
2 tablespoons hummus
See more foods in the protein group.
Dairy
Consuming dairy helps older adults maintain strong bones and provides several vital nutrients, including calcium, potassium, and vitamin D. For your heart health, pick from the many low-fat or fat-free choices in the dairy group. These give you important vitamins and minerals, with less fat. Certain fortified dairy alternatives can provide similar nutritional content to dairy.
1 cup-equivalent of dairy equals:
1 cup yogurt
1-1/2 ounces hard cheese, such as cheddar, mozzarella, Swiss, or Parmesan
1/3 cup shredded cheese
1 cup milk or calcium-fortified soy beverage
2 cups cottage cheese
1 cup pudding made with milk
See more foods in the dairy group.
Other foods
Some foods are not in any of the main food groups. These include oils, which can be eaten regularly as part of a healthy diet, as well as unhealthy fats, sugars, and calories from drinks, which should only be consumed occasionally. There is no recommended daily intake amount in cups or ounces for these products. Limiting the calories you consume from this category can help keep your healthy eating habits on track.
Oils & solid fats
Oils are high in calories, but they are also an important source of nutrients like vitamin E. For older adults, the daily allowance of oils ranges from 5 to 8 teaspoons, depending on activity level. Oils contain monounsaturated and polyunsaturated fats, which are healthy fats that give you energy and help the body absorb certain vitamins.
Measuring your daily oils can be tricky — knowing what you add while cooking or baking is one thing, but oil is naturally a part of some foods.
Teaspoons of oil:
1/2 medium avocado has 3 teaspoons of oil
4 large ripe olives have 1/2 teaspoon of oil
1 tablespoon of peanut butter has 2 teaspoons of oil
See more oil equivalents.
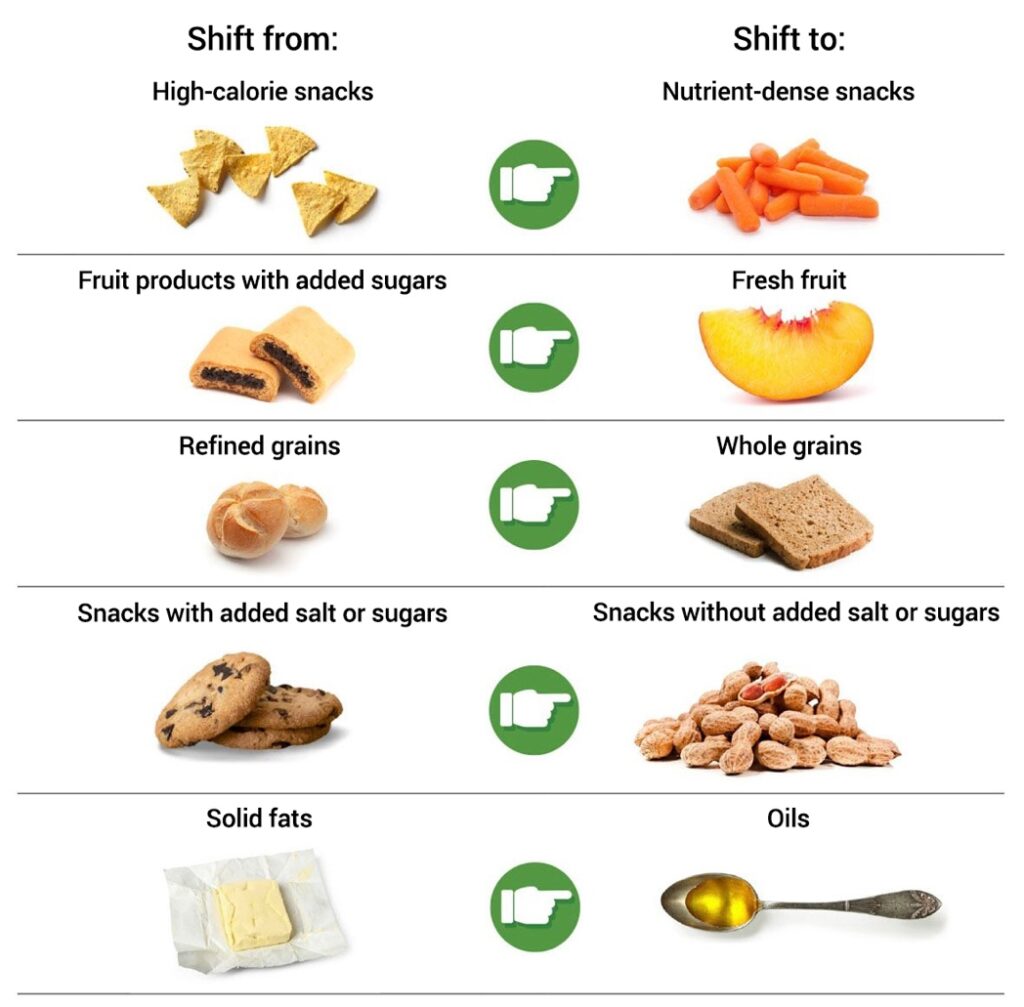
In general, try to use oils instead of solid fats, such as butter or lard, which are high in saturated fat. Saturated fats occur naturally in some foods, but they are also added to foods such as baked goods and potato chips. To lower the saturated fat in your diet, eat low-fat or fat-free dairy products, choose cuts of meat with less fat, and remove the skin from chicken. Reading the Nutrition Facts label can help you keep track of how much saturated fat you consume.
Limit the consumption of foods high in added sugar, which include sweetened cereals, highly processed snack foods such as cookies and cakes, dairy desserts, and many items marketed as low-fat. Read the ingredient list to see if the food you are eating has added sugar. Some key words to look for: brown sugar, corn sweetener, corn syrup, dextrose, fructose, and high-fructose corn syrup.
Beverages
Although many beverages can be part of a healthy eating pattern, some add calories without adding nutritional value and you should avoid them. Beverages that are calorie-free — especially water — or that contribute beneficial nutrients, such as fat-free and low-fat milk and 100% juice, should be the primary beverages you consume.
Coffee and tea. Drinking coffee or tea barely provides any calories unless you add sugar or cream, which are not nutrient-dense and should be consumed in moderation. Be cautious when ordering drinks from coffee shops because these are often loaded with extra sugars and fats.
Sweetened beverages. Examples of beverages that often have added sugars are soda, fruit drinks, sports drinks, energy drinks, and sweetened waters. Most sweetened beverages do not contribute to meeting food group goals and often contain a high number of calories.
Alcohol. Alcohol is not nutrient-dense and is not part of the healthy eating patterns recommended in the Dietary Guidelines. If you consume alcohol, do so in moderation, defined as one drink or less per day for women and two drinks or less per day for men.
Calories from sugars, saturated fats, and drinks can add up quickly. As these foods provide no nutritional benefit, they should only be consumed on occasion and in limited amounts.
To learn more, please visit https://www.nia.nih.gov/health/healthy-eating-nutrition-and-diet/healthy-eating-you-age-know-your-food-groups.