Taking care of yourself is one of the most important things you can do as a caregiver. Caregiving is not easy — not for the caregiver and not for the person receiving care. It requires sacrifices and adjustments for everyone. Often, family caregivers must juggle work and family life to make time for these new responsibilities.
Caring for an older adult can also be rewarding. Many people find that caregiving provides a sense of fulfillment and that they like feeling useful and needed. But the ongoing demands of taking care of someone else can strain even the most resilient person. That’s why it’s so important for you to take care of yourself. This article can help you find ways to look out for your own well-being so you can be there for others.
How do you know if you need help?
Caregivers do a lot for others. Because there is so much on their plate, many caregivers don’t spend time taking care of themselves. For example, they are less likely than others to get preventive health services, like annual checkups, and to practice regular self-care. As a result, they tend to have a higher risk of physical and mental health issues, sleep problems, and chronic conditions such as high blood pressure. They are even at an increased risk of premature death.
It’s not always obvious when a person needs help. Watch out for these signs of caregiver stress:
- Feeling exhausted, overwhelmed, or anxious
- Becoming easily angered or impatient
- Feeling lonely or disconnected from others
- Having trouble sleeping or not getting enough sleep
- Feeling sad or hopeless, or losing interest in activities you used to enjoy
- Having frequent headaches, pain, or other physical problems
- Not having enough time to exercise or prepare healthy food for yourself
- Skipping showers or other personal care tasks such as brushing your teeth
- Misusing alcohol or drugs, including prescription medications
Don’t wait until you are completely overwhelmed. Learn what your own warning signs are and take steps to minimize sources of stress where possible.
How can you ask others to help?
When people have asked you if they can lend a hand, have you told them, “Thanks, but I’m fine”? Accepting help from others isn’t always easy. You may worry about being a burden, or you may feel uncomfortable admitting that you can’t do it all yourself. But many caregivers later say they did too much on their own, and they wished they had asked for more support from family and friends.
Understand that many people want to help, and it makes them feel good to contribute. If asking for help is hard for you, here are some tips that may help:
- Ask for small things at first, if that makes it easier for you. Many large jobs can be broken down into simpler tasks.
- If you aren’t comfortable asking face-to-face, send a text or email with your request.
- Consider a person’s skills and interests when thinking about how they could help.
- Be prepared with a list of things that need to be done, and let the other person choose what they’d like to do.
- If someone offers to help, practice saying, “Thanks for asking. Here’s what you can do.”
- Be honest about what you need and what you don’t need. Not every offer is going to be helpful.
- Be prepared for some people to say “no,” and don’t take it personally.
What else can a caregiver do if they’re feeling overwhelmed?
If you’re feeling overwhelmed by caregiving, tending to your own needs may be the last thing on your mind. But taking time for yourself can actually make you a better caregiver. If you can find small ways to lower your stress and boost your mood, you’ll have more strength and stamina to take care of someone else.
Below are some suggestions that may help when you’re feeling overwhelmed. Remember that you don’t have to do everything all at once, especially if the thought of self-care just makes you feel more exhausted.
- Be active. Find something active that you enjoy. That might be walking, dancing, gardening, or playing with a pet. Even short periods of exercise can be beneficial.
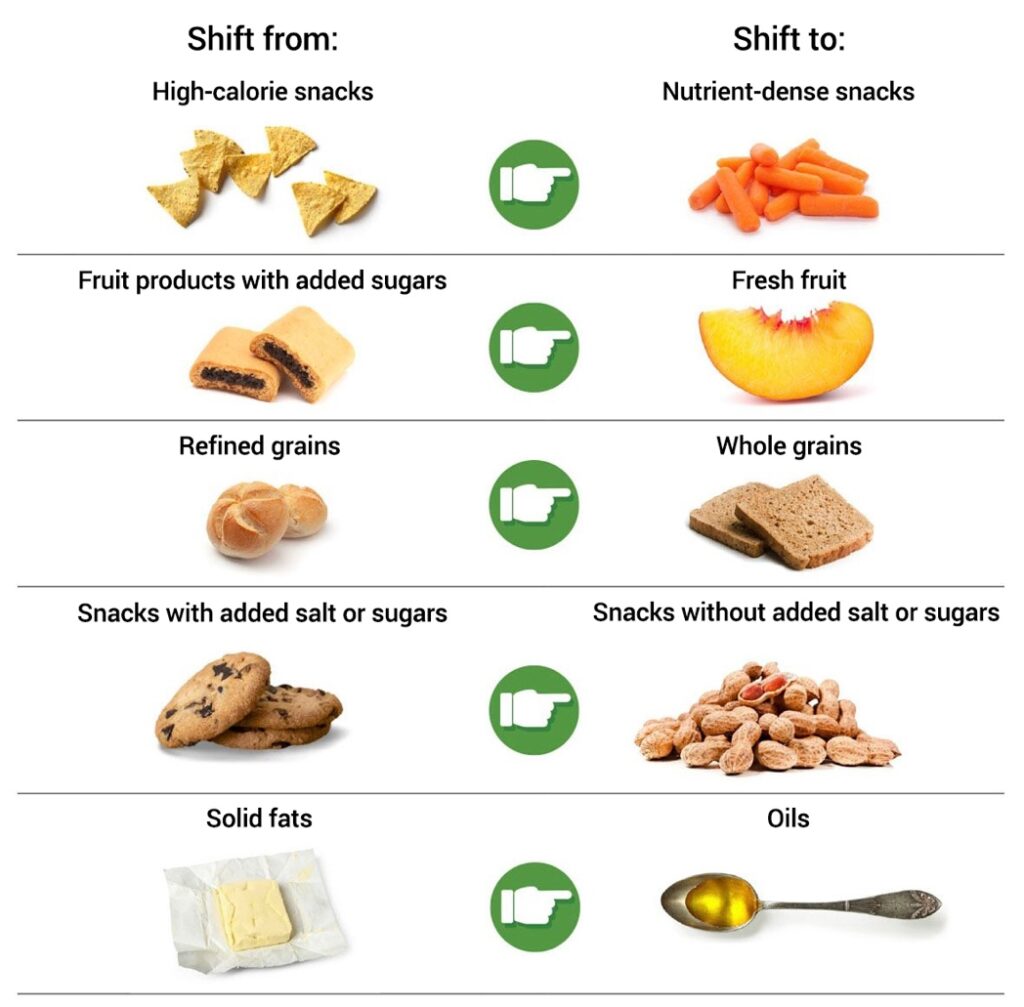
- Eat well. Work on having a well-balanced diet that includes a variety of healthy foods. Drink plenty of water every day.
- Prioritize sleep. Aim to get seven to nine hours of sleep each night. Develop a relaxing bedtime routine to make it easier to fall asleep. Try to go to sleep and get up at the same time each day.
- Reduce stress. Experiment with relaxation techniques like meditation, tai chi, or yoga. Download a smartphone app with guided meditations or relaxing music. Many of these apps are free.
- Make time to relax. Carve out time each week to do something you enjoy that has nothing to do with caregiving. It can be as simple as watching a favorite TV show, reading a magazine, or working on a hobby.
- Keep up with your own health. Make that doctor’s appointment you’ve been putting off. Tell your doctor that you’re a caregiver: They may be able to suggest resources online or in your community.
- Reach out for support. Talk to a trusted family member or friend or seek counseling from a mental health professional. Join an online or in-person support group for caregivers. These are people who will know what you’re going through and may have suggestions or advice.
- Take a break if you need it. Ask another family member or friend to step in, hire an aide to come for a few hours a week, or sign up the older person for an adult day care program.
- Be kind to yourself. You don’t have to pretend to be cheerful all the time. Feelings of sadness, frustration, and guilt are normal and understandable. Express your feelings by writing in a journal or talking with a friend.
Remember that you are doing the best you can and that you are not alone. Many caregivers have trouble tending to their own health and well-being. But give yourself credit for everything you’re doing. Your caregiving makes a big difference in someone else’s life.
If you’re not the primary caregiver, how can you support that person?
In many cases, one person takes on most of the everyday responsibilities of caring for an older person. It tends to be a spouse or the child or sibling who lives closest. If you are not the primary caregiver, you can still play an important role in supporting that person.
Be sure to acknowledge how important the primary caregiver is in the older person’s life. Also, discuss the physical and emotional effects caregiving can have on people. Although caregiving can be satisfying, it also can be very hard work.
You can lighten the primary caregiver’s load by providing emotional support, taking on specific tasks, and even providing full-time care for a short period of time to give the primary caregiver a break. Ask them what you can do that would be most helpful. Staying in contact by phone or email might also take some pressure off the primary caregiver. Just listening may not sound like much, but it can mean a lot.
A primary caregiver — especially a spouse or partner — may be hesitant to ask for a break. Here are some ways you could help them get the rest they need:
- Offer to stay with the older person for one afternoon a week, for example, so the primary caregiver can have some personal time.
- Arrange for regular respite care in the form of a volunteer, an in-home aide, or an adult day care program.
- If you live far away, travel to stay with the older person for a few days so the primary caregiver can take a vacation or just have some time off.
In time, the older person may have to move to a residential (live-in) facility, such as assisted living or a nursing home. If that happens, the primary caregiver will need your support. You can work together to select a facility and coordinate the move. The primary caregiver may need extra support while adjusting to the person’s absence and to living alone at home. To learn more, please visit https://www.nia.nih.gov/health/caregiving/taking-care-yourself-tips-caregivers.